Consumer Resource Hub
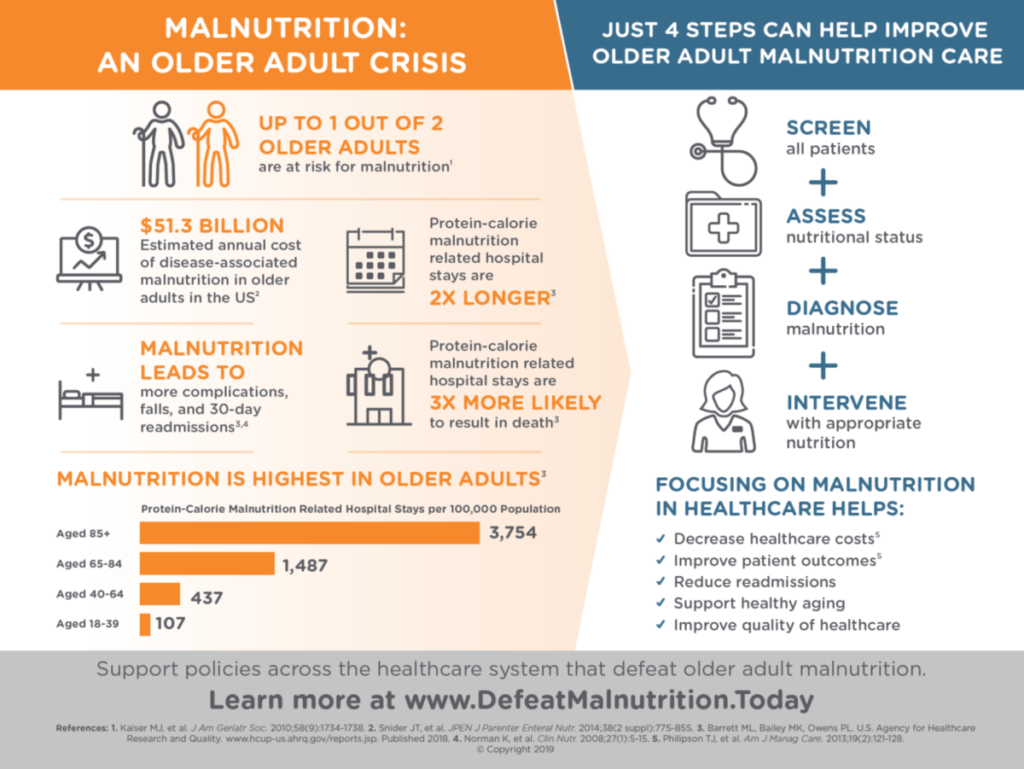
Up to 1 out of 2 older Americans are at risk for malnutrition. The numbers are even higher for older adults in health care settings. About 60% of older adults in hospitals and 35-85% of older residents in long-term care facilities are malnourished. Malnutrition can worsen chronic conditions and make it difficult for older adults to remain independent. Malnutrition can result from multiple factors, including food insecurity, chronic disease, and/or inequality in social determinants of health.
Nearly every community has programs to help older adults get the nutrition they need. But many older adults and their caregivers—and even many doctors and hospitals—may not know about the programs or how to connect with them. This Resource Hub includes practical resources, tools, and ideas to help you identify malnutrition whether resulting from food insecurity or other factors and develop nutrition plans for yourself and others.
The original content was developed in conjunction with the Maryland Department of Aging, Defeat Malnutrition Today, Meals on Wheels America, Brandman Centers for Senior Care, and a panel of expert reviewers. Updated content was developed by Defeat Malnutrition Today. Support was provided by Abbott Nutrition, a division of Abbott.
UNDERSTANDING THE RISK FACTORS LIKE FOOD INSECURITY AND CHRONIC DISEASE CAN HELP US SPOT AND ADDRESS MALNUTRITION.
Malnutrition: A Hidden Epidemic Among Older Adults video below from Alliance for Aging Research (2016) gives an overview of malnutrition among older adults. Also available in Spanish.
This video below from Defeat Malnutrition Today (2016) makes the case for policy makers to address malnutrition through a nutrition protocol (Spanish)
Malnutrition: An Older Adult Crisis graphic below from Defeat Malnutrition Today (2019) explains healthcare costs associated with malnutrition
Oral Nutrition Supplements from Dietitian Connection (2020) explains how oral nutritional supplements (ONS) can help malnutrition, and offers examples of ONS products for malnourished adults.
This infographic from the American Society for Parenteral and Enteral Nutrition (ASPEN) (2021) describes the causes of older adult malnutrition and what it means to have good nutrition.
Health equity means that every person has an opportunity to be as healthy as possible. For many communities, structural barriers to health like poverty and discrimination limit access to nutritious food, safe and convenient transportation, and housing. Even with the most equitable approach, groups experiencing health disparities have further to go to attain their full health potential.
To promote health equity, we can advocate for continued support of government programs like the Supplemental Nutrition Assistance Program (SNAP) and older adult congregate and home-delivered meal programs like Meals on Wheels.
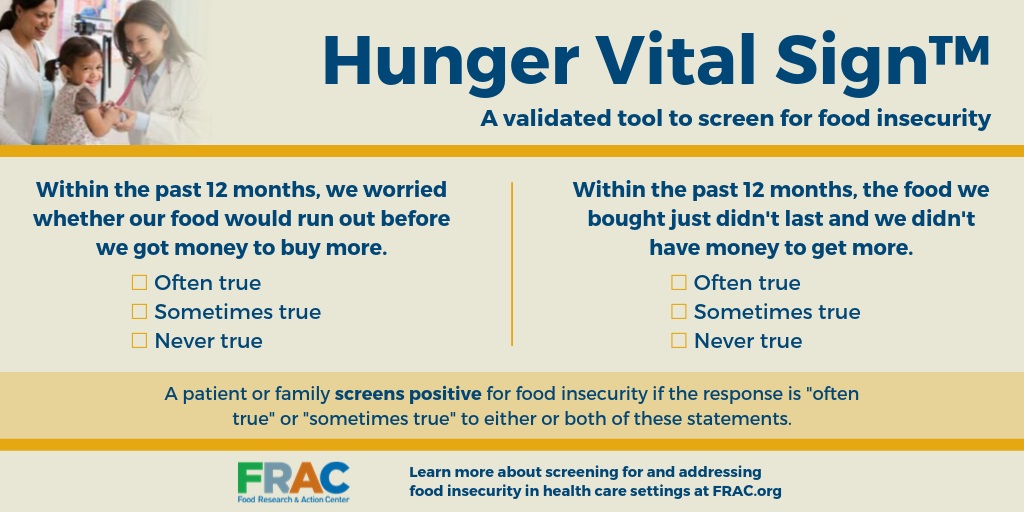
Another way to help promote health equity is to screen everyone for food insecurity and malnutrition.
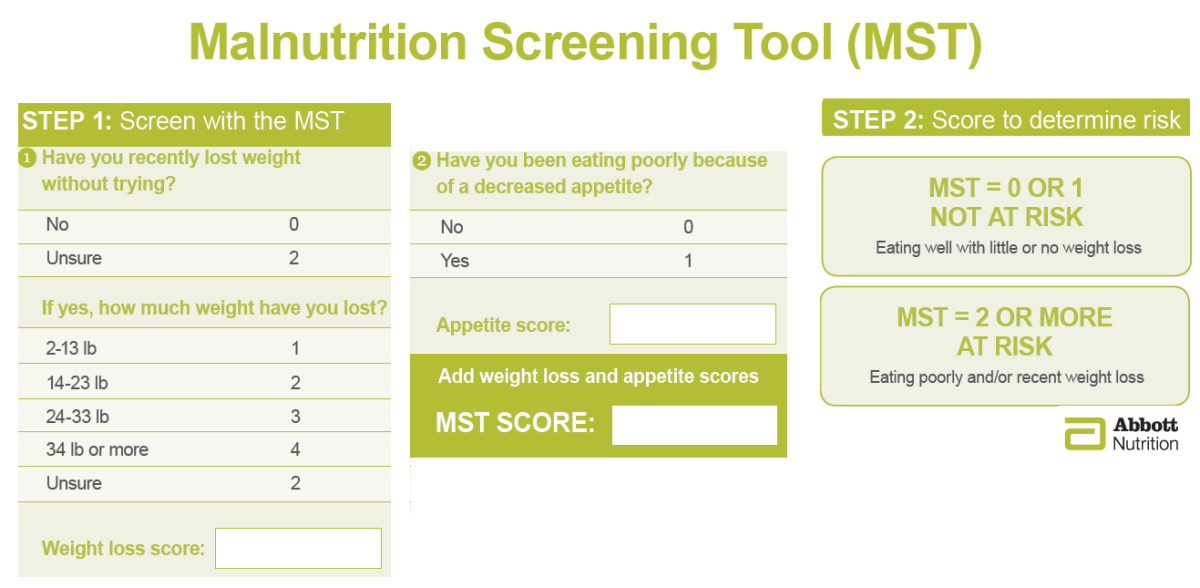
THE TWO ITEM MALNUTRITION SCREENING TOOL:
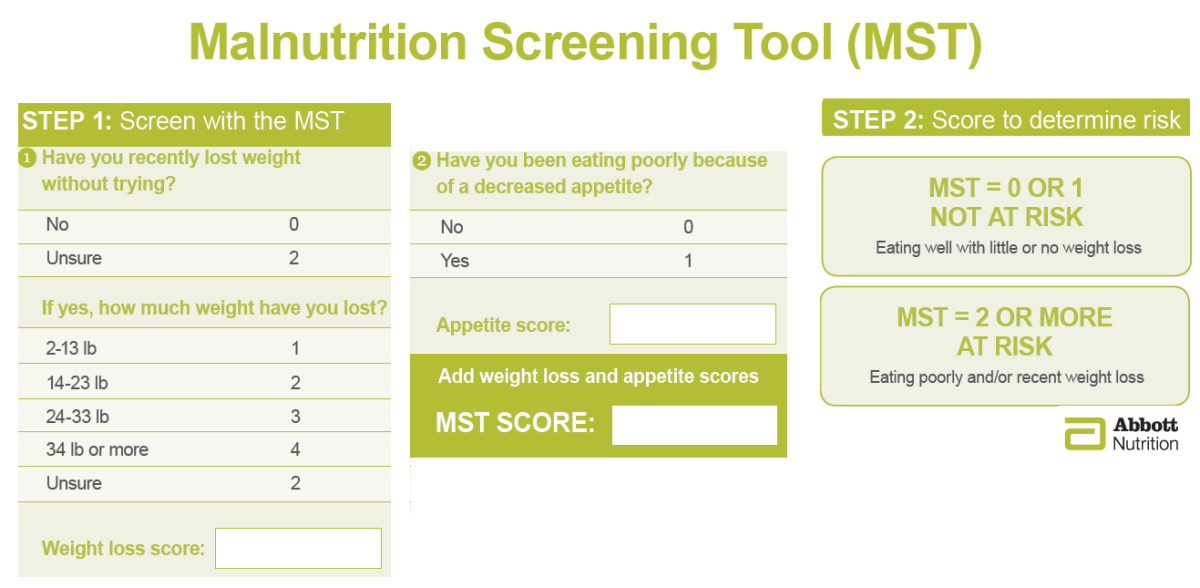
ONE SIMPLE WAY TO HELP IDENTIFY MALNUTRITION IS TO USE THE MALNUTRITION SCREENING TOOL
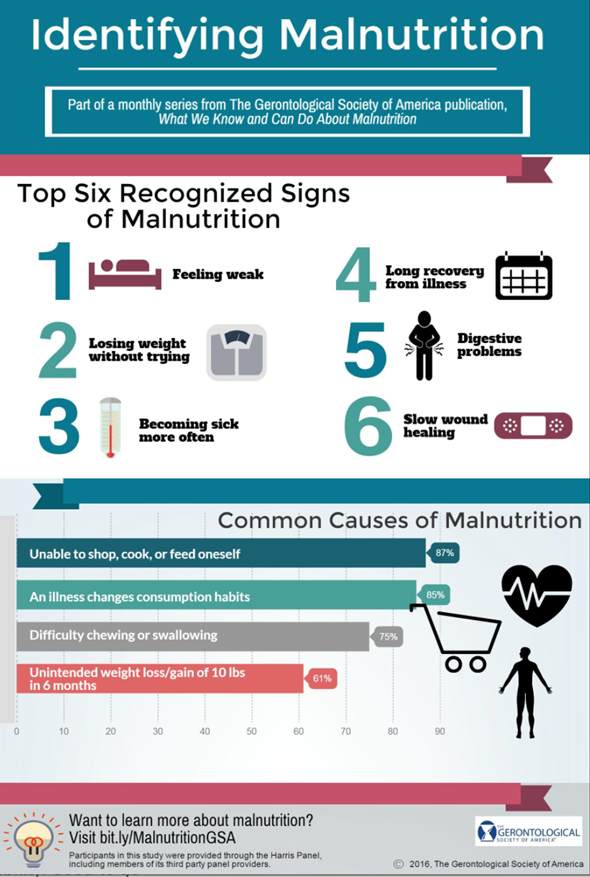
Identifying Malnutrition from the Gerontological Society of America (GSA) (2016) describes the top 6 signs of malnutrition and common causes
TALK TO YOUR HEALTHCARE PROVIDER ABOUT YOUR CONCERNS ABOUT MALNUTRITION.
This short video below and infographic from the American Society for Parenteral and Enteral Nutrition (ASPEN) (2019) will help you and your loved ones talk with your healthcare providers about nutrition.
Closer look at hidden impact of malnutrition and the hidden impact of a poor diet from the Canadian Malnutrition Taskforce (2019) show signs of malnutrition and suggest tips for addressing malnutrition.
Understanding Food Insecurity
- Food insecurity exists whenever it’s difficult to access nutritionally adequate, safe, and acceptable food in a socially acceptable way. We look at the 5 A’s to determine if someone is food insecure. When one or more of these Five A’s are not met, then a person can fall into food insecurity. (Check out The Food Security Quest to learn more)
- Availability: Sufficient food for all people at all times
- Accessibility: Physical and financial access to food at all times (can you get there? Is it far? Is it affordable?)
- Adequacy: Access to food that is nutritious and safe (Is there healthy food there?)
- Acceptability: Access to culturally acceptable food, produced and obtained in ways that do not compromise people’s dignity (Is there stigma around accepting food? Are these foods you commonly eat?)
- Agency: The local and national policies, groups, and programs that help you achieve food security (ex. SNAP, food pantries, school lunch)
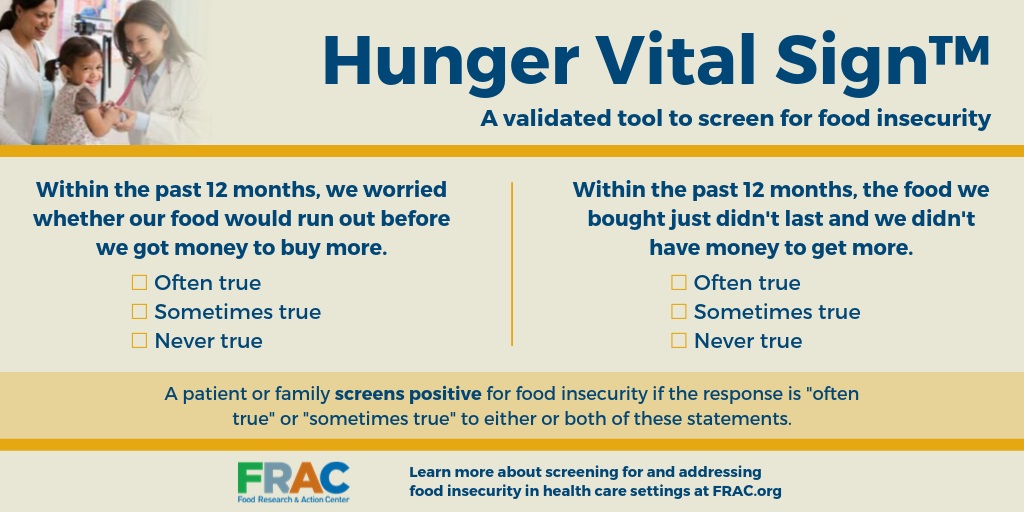
Answering the Two Item Food Insecurity Screening Questions can help decide if someone is food insecure
Groups with higher than average rates of food insecurity in 2019 were
- Households with incomes near or below the Federal Poverty Line
- Households with children
- Single Parents
- Black and Hispanic households
- People living alone
- Disability, physical limitations, and chronic health conditions
- Geography -urban, rural, and low-income areas can be far from grocery stores or lacking in fresh produce sales
- Employment-both being unemployed and being employed but in a low-wage job
- Housing and Transportation-Lack of access to either
- Structural inequality, policy, and discriminatory practices put some populations of individuals at higher risk for food insecurity.
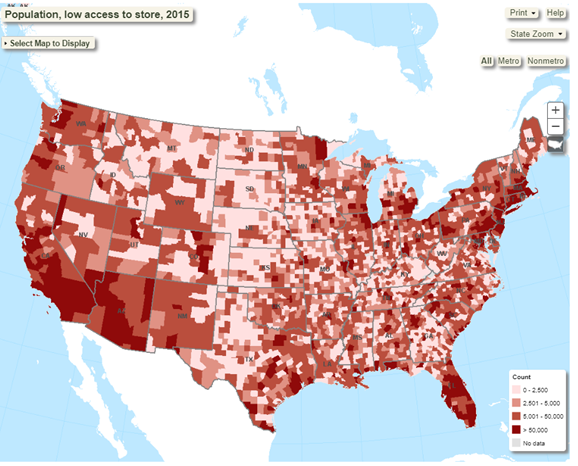
Did you know predominantly white neighborhoods have four times more grocery stores than Black neighborhoods. The USDA food environment atlas(link is external) can show you national and local data like the map below
Click in the Nutrition Assistance Programs to learn more about food and nutrition programs like SNAP

Nutrition Assistance Programs
There are several different nutrition programs for older adults, including meals programs as well as food programs. Some are government programs that provide meals like home-delivered and congregate meals. These are specifically focused for adults 60+ years old and available irrespective of income levels. Some provide groceries, like non-government food pantries and food banks and often don’t require proof of income. Some programs provide money for food and are limited by income level, like the Supplemental Nutrition Assistance Program (SNAP):
MEALS PROGRAMS
- Eldercare Locator(link is external) helps you find local programs
- Home Delivered Meals: Like Meals on Wheels(link is external), they deliver meals to seniors in need.
- Congregate Meals: provide group meals and socialization for all seniors, regardless of need (see map below)
- Other programs to look for in your area (availability varies by state)
- Food is Medicine programs
- Some Medicare Advantage insurances include meals benefits
- Check if your local hospital has a food pharmacy
OLDER AMERICANS ACT NUTRITION SERVICES
The Older Americans Act (OAA) helps support social and nutrition services for older adults. OAA nutrition programs are congregate (senior center) meals and Meals on Wheels. This map has links to each state's OAA programs.
OLDER AMERICANS ACT NUTRITION SERVICES
The Older Americans Act (OAA) helps support social and nutrition services for older adults. OAA nutrition programs are congregate (senior center) meals and Meals on Wheels. This map has links to each state's OAA programs.
SUPPLEMENTAL NUTRITION ASSISTANCE PROGRAM (SNAP)
This map has links to each state's SNAP application.
Eating and drinking a balanced diet can help your body cope with treatment side effects and heal faster.
CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD)
Reduced food intake is common, and energy and protein needs are often increased making eating enough difficult. You can better your nutrition to prevent malnutrition
These infographics low risk, medium risk, high risk from UK’s Malnutrition Pathway (2020) give nutrition advice based on malnutrition risk level
CANCER
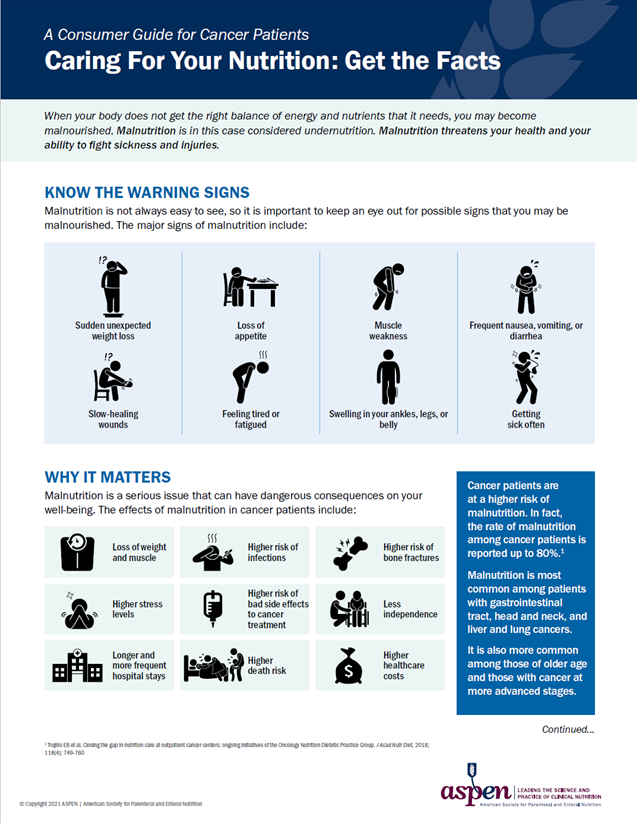
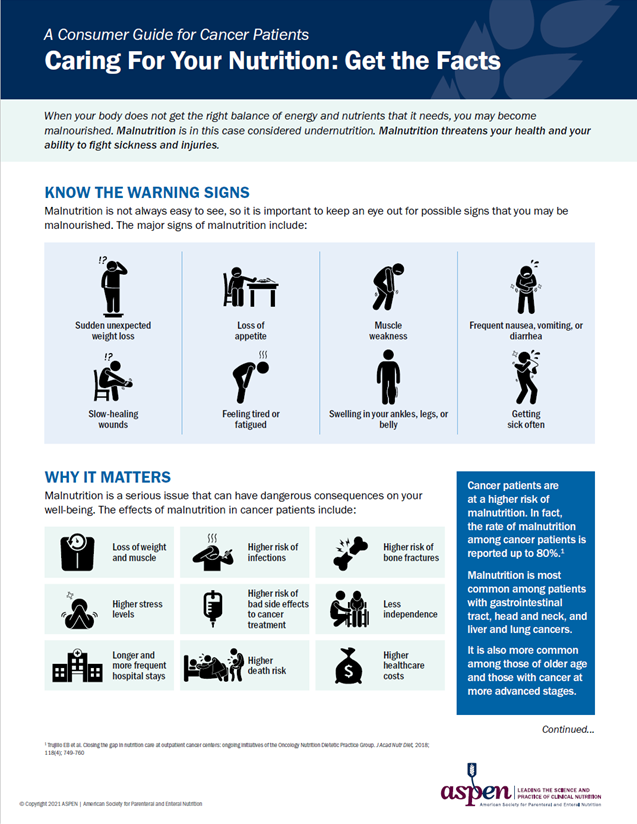
Malnutrition is one of the most common side effects of cancer and treatment side effects and can affect up to 80% of patients depending on tumor type and stage, according to NCI.
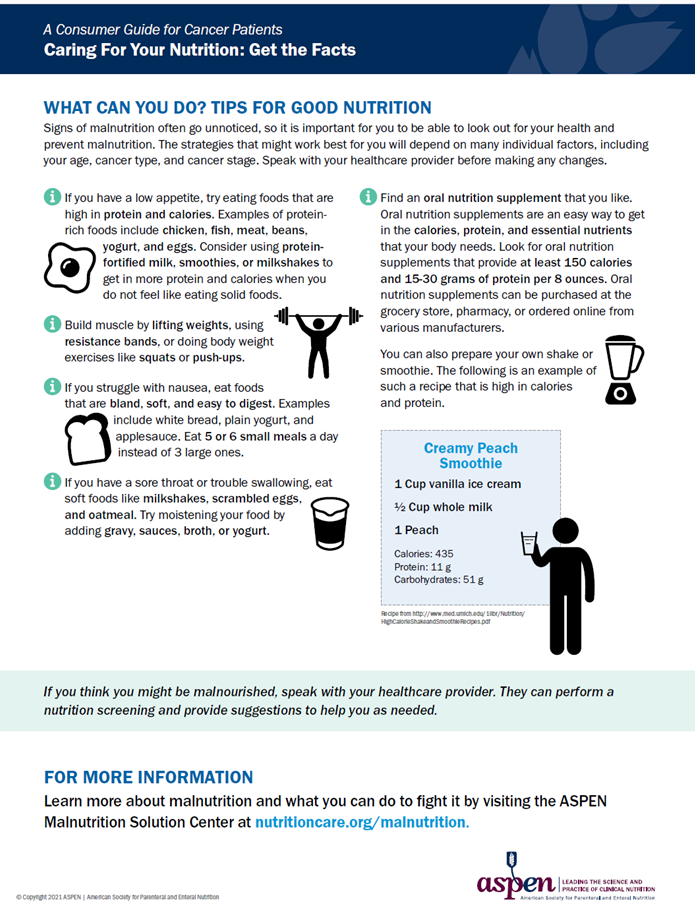
The Consumer Guide for Cancer Patients-Caring for your Nutrition from the American Society on Parenteral and Enteral Nutrition (ASPEN) (2021) helps you spot the signs and can help you focus on ways to better your nutrition
DIABETES
Diabetic complications like gastroparesis (food moves slowly through gut) and ketoacidosis (very high blood sugar and ketones in blood) can lead to a poor appetite and increased risk of malnutrition. A 2018 study found 16.5% of older adults with diabetes on Medicare had protein-energy malnutrition and they had a 69% increased risk of dying as compared to older adult diabetics on Medicare without malnutrition.
This High protein, high energy eating and diabetes from the Australian Diabetes Association (2017) gives tips for diabetic high protein, high calorie meals when you have a poor appetite. Look here for more tips on preventing unintentional weight loss in diabetes.
ORAL NUTRITION SUPPLEMENTS
Oral Nutrition Supplements from Dietitian Connection (2020) explains how oral nutritional supplements (ONS) can help malnutrition and offers examples of ONS products for malnourished adults.
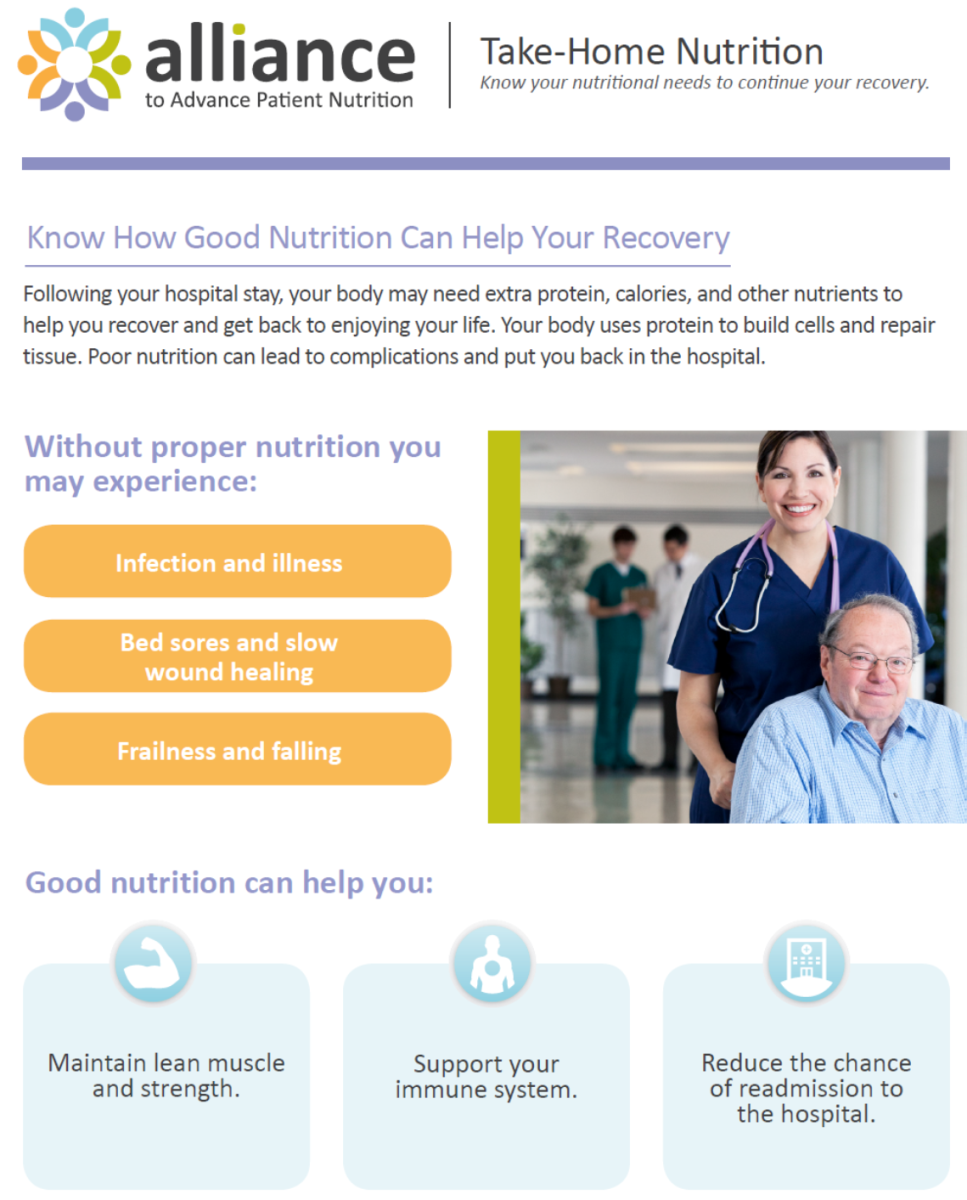
Surgery and hospitalization are stressful events for your body, and a highly nutritious diet helps you prepare and supports your recovery in many ways.
Preventing Malnutrition After a Hospital Stay: 6 Questions to Ask Your Doctor (2016) from the National Council on Aging (NCOA) offers tips on how older adults entering the hospital can plan ahead to get the nutrition they need during their hospital stay and when they return home.
6 Questions to Ask your Doctor
- What is my current nutritional status?
- How can I make sure to eat well when I get home?
- How will I know if I'm becoming malnourished?
- How should I manage my prescribed medications?
- Which foods should I eat and which should I avoid as I recover?
- Should I avoid physical activity, and if so, for how long?
The Enhanced Recovery After Surgery (ERAS, 2020) from Defeat Malnutrition Today helps ensure the best possible outcomes after surgery. Many healthcare providers are helping people improve their nutrition before and after an elective procedure by following Enhanced Recovery After Surgery (ERAS®) care plans. Learn more about ERAS care plans (here) and ERAS nutrition strategies (here)
Importance of muscle mass in recovery: Sarcopenia is an advanced form of muscle loss. this easy-to-understand video (Spanish video) by Aging in Motion (2021) explains Sarcopenia and Sarcopenia Facts and Figures shows consequences of muscle loss.
Post-hospital Recovery: Know How Good Nutrition Can Help Your Recovery from the Alliance to Advance Patient Nutrition (2014) highlights the importance of nutrition and reviews tips to help adults avoid malnutrition after discharge.

Eating healthy foods can help prevent many health problems as you age, such as heart disease, stroke, diabetes, and obesity.
- Choosing Healthy Meals as You Get Older from the National Institute of Aging provides 10 healthy eating tips for people 65+.
- Smart Food Choices for Healthy Aging from the National Institute on Aging is an interactive website to teach you about key nutrients, portion sizes, food labels, as an older adults plus tips for eating well on a budget
- Diet and Exercise: Choices Today for a Healthier Tomorrow (Spanish) from the National Institute on Aging on easy ways to age well!
- Build a Healthy Eating Routine as You Get Older from the US Dietary Guidelines (2021) details tips to build a healthy routine.
- Your Guide to Making the Most of Your Food from UK’s Malnutrition Pathway (2021) provides simple ideas on how you can get the most nutrition from food, even when you’re not feeling your best
- How to stay hydrated for optimal health ;from the National Council on Aging (2021) explains why it’s even more important to stay hydrated as you get older.
- What Your Protein Habits Say About Your Health -this 2019 study found that one in three adults over the age of 50 have insufficient daily protein intake. Read this article to see if you’re meeting your protein goals.
Meal Planning
Meal planning takes the guesswork out of eating and can help ensure you eat a variety of nutritious foods throughout the day.
- The SNAP program has meal planning tips for those on a budget
- Healthy Meal Planning: Tips for older adults from the National Institute on Aging helps you answer “what should I eat?”
- MyPlate for older adults from the US Department of Agriculture is based on the 2020 Dietary Guidelines and offers healthy eating tips for aging well. Take this quiz to get personalized recommendations.
- Download the Myplate App for
- Goal Setting (you can use your quiz results)
- Real-time progress
- Badges and challenges
- Tips for reaching nutrition goals
- Recipes

- This benefits checkup from the National Council on Aging (NCOA) identifies local programs that you may qualify for.
- Elder Index from Gerontology Institute (2021) is a tool to identify local expenses, savings requirements, and what incomes are needed to achieve economic security by family type, and at the city, county, and state levels.
- What do we Know and Can Do about Malnutrition from the Gerontological Society of America (GSA) (2015) surveyed Americans to measure their knowledge and perceptions about malnutrition in older adults. Key Findings: Americans understand that identifying and treating malnutrition is important for older adult health and would like more information on the problem.
- Managing Muscle Loss: What You Need to Know report from AARP/Abbott (2016) provides insights into the state of health for AARP members age 50+, as well as this group’s understanding of important nutrition, exercise, and muscle mass fundamentals.
